Introduction
Idiopathic Pulmonary Fibrosis (IPF) and Progressive Pulmonary Fibrosis (PPF) are two of the most challenging conditions in respiratory medicine, significantly impacting the quality of life of those affected. IPF, a specific form of chronic, progressive fibrosing interstitial pneumonia, predominantly affects older adults and is marked by the histopathologic and/or radiologic pattern of usual interstitial pneumonia (UIP). PPF, encompassing various types of interstitial lung diseases (ILDs), is characterized by progressive scarring and worsening lung function. This webpage delves into the intricacies of IPF and PPF, offering insights into their definitions, diagnostic criteria, and treatment methodologies, all based on the latest guidelines.
About IPF
Definition and Diagnostic Criteria of IPF
- Definition: IPF is characterized as a distinctive type of chronic, progressive fibrosing interstitial pneumonia, the origins of which remain unknown, predominantly affecting older adults. This condition, confined to the lungs, presents with a histopathologic and/or radiologic pattern indicative of usual interstitial pneumonia (UIP).
- Diagnostic Criteria: The diagnosis of IPF requires a comprehensive approach, involving a detailed assessment of the patient’s clinical history, radiological findings, and, in some cases, histopathological examination.
a. Exclusion of other known causes of interstitial lung disease (ILD) (e.g., domestic and occupational environmental exposures, connective tissue disease, and drug toxicity).
b. The presence of a UIP pattern on high-resolution computed tomography (HRCT) in patients not subjected to surgical lung biopsy.
c. Specific combinations of HRCT and surgical lung biopsy pattern in patients subjected to surgical lung biopsy.
Raghu et al., Am J Respir Crit Care Med. 2011;183(6):788–824
Diagnostic algorithm for IPF
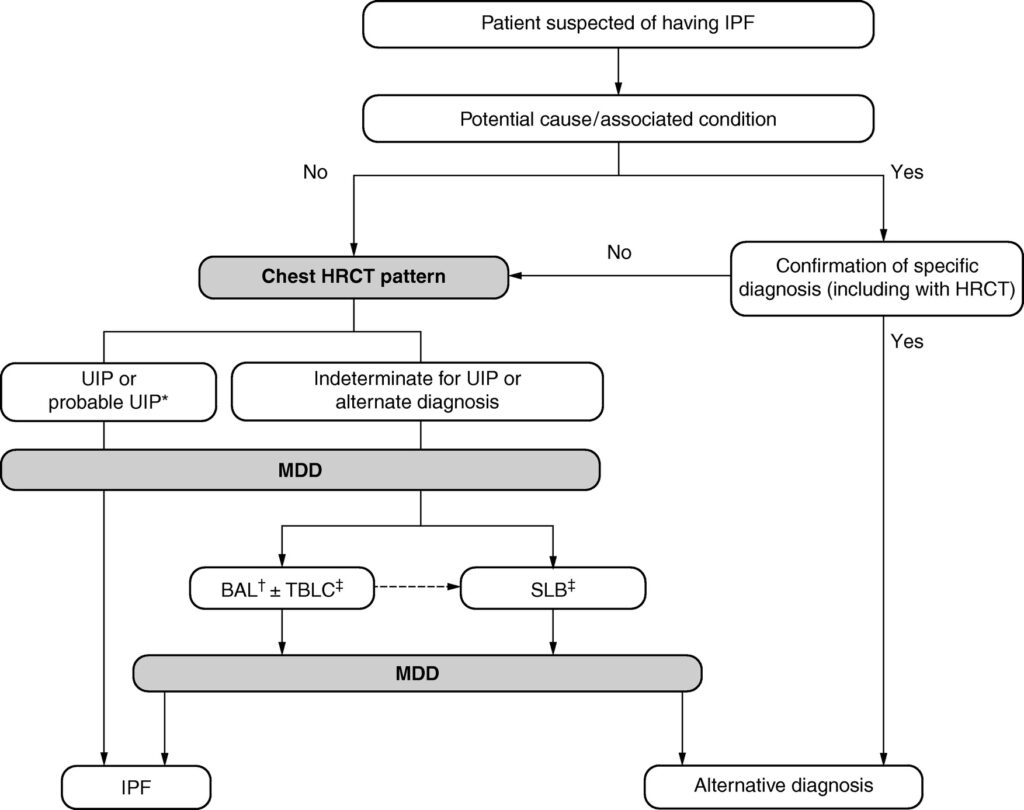
Raghu et al., Am J Respir Crit Care Med 2022;205:e18–e47
Treatment Methods
- Pharmacological Treatments
- Nintedanib: This oral medication acts as a tyrosine kinase inhibitor, effectively blocking the pathways involved in the fibrogenesis process. It’s one of the primary drugs recommended for managing IPF, known to slow disease progression.
- Pirfenidone: Another key oral medication for IPF, Pirfenidone, has anti-inflammatory, antioxidative, and antiproliferative properties. It plays a significant role in managing the symptoms and progression of IPF.
- Non-Pharmacological Treatments
- Oxygen supplementation is crucial for patients experiencing low blood oxygen levels (hypoxemia). It helps alleviate symptoms and improve quality of life.
- Pulmonary rehabilitation programs are recommended to enhance physical conditioning, reduce symptoms, and improve overall well-being.
Mechanism of Action of Nintedanib and Pirfenidone
- Nintedanib: Targets and inhibits multiple tyrosine kinases involved in the fibrotic process, thereby reducing fibrogenesis and slowing down the disease progression.
- Pirfenidone: It works by reducing lung fibrosis through its anti-inflammatory, antioxidative, and antiproliferative effects. This multifaceted approach helps control the progression of IPF.
About PPF
Definition and Diagnostic Criteria of PPF
- Definition: PPF includes a spectrum of ILDs that are marked by progressive scarring and a gradual decline in lung function. Unlike IPF, PPF can arise from various underlying conditions.
- In a patient with ILD of known or unknown etiology other than IPF who has radiological evidence of pulmonary fibrosis, PPF is defined as at least two of the following three criteria occurring within the past year with no alternative explanation
- Diagnostic Criteria: The diagnosis of PPF involves a thorough evaluation of the patient’s medical history, symptoms, and lung function tests.
1. Worsening respiratory symptoms
2. Physiological evidence of disease progression (either of the following):
a. Absolute decline in FVC ⩾5% predicted within 1 yr of follow-up
b. Absolute decline in DlCO (corrected for Hb) ⩾10% predicted within 1 yr of follow-up
3. Radiological evidence of disease progression (one or more of the following):
a. Increased extent or severity of traction bronchiectasis and bronchiolectasis
b. New ground-glass opacity with traction bronchiectasis
c. New fine reticulation
d. Increased extent or increased coarseness of reticular abnormality
e. New or increased honeycombing
f. Increased lobar volume loss
Raghu et al., Am J Respir Crit Care Med 2022;205:e18–e47
Treatment Methods
- The treatment of PPF is multifaceted, often involving the use of antifibrotic agents such as Nintedanib and Pirfenidone. Supportive care, including oxygen therapy and pulmonary rehabilitation, is also critical in managing the symptoms and improving the quality of life of patients with PPF.
Reference Links
- An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline
- An Official ATS/ERS/JRS/ALAT Statement: Idiopathic Pulmonary Fibrosis: Evidence-based Guidelines for Diagnosis and Management