Introduction
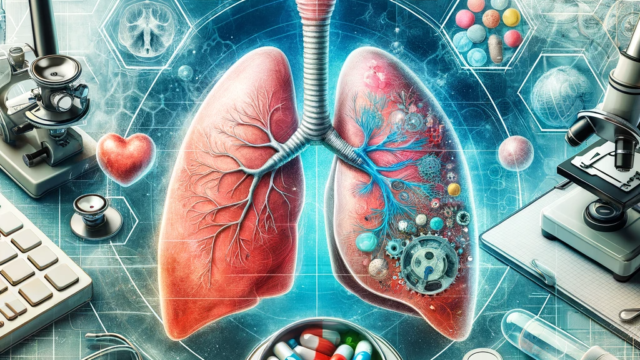
Chronic Obstructive Pulmonary Disease (COPD) and Pulmonary Fibrosis are two of the most prevalent lung diseases, significantly impacting global health. While COPD is characterized by obstructed airflow from the lungs, Pulmonary Fibrosis involves the thickening and scarring of lung tissue. Understanding the interrelation between these diseases and the advancements in clinical trials is critical for developing effective treatments.
Part 1: Understanding COPD and Pulmonary Fibrosis
COPD
Pathophysiology
COPD develops due to chronic inflammation in the lungs, leading to obstructed airflow. Key factors include smoking, environmental pollutants, and genetic predisposition. The disease is marked by symptoms like chronic cough, shortness of breath, and frequent respiratory infections.
Risk Factors and Symptoms
Smoking is the primary risk factor for COPD. Other factors include exposure to air pollutants, occupational dust, and a history of frequent lung infections. Symptoms often include breathlessness, chronic cough, wheezing, and fatigue.
Current Standard Treatments
Treatment for COPD typically involves bronchodilators, corticosteroids, and pulmonary rehabilitation. Smoking cessation is also crucial. While these treatments can manage symptoms, they cannot reverse the damage to lung tissue.
Pulmonary Fibrosis
Pathophysiology
Pulmonary Fibrosis involves the progressive scarring of lung tissue, leading to a decline in lung function. The exact cause is often unknown, but factors like environmental exposure and certain medications can contribute.
Causes and Symptoms
The causes of Pulmonary Fibrosis can range from environmental factors like exposure to certain chemicals to medical treatments like radiation therapy. Symptoms include a persistent dry cough, fatigue, and shortness of breath.
Treatment Approaches
Treatments focus on slowing the disease progression and improving quality of life. Medications like antifibrotic agents and anti-inflammatory drugs are commonly used, along with oxygen therapy and pulmonary rehabilitation.
Part 2: The Interrelation between COPD and Pulmonary Fibrosis
The interrelation between COPD and Pulmonary Fibrosis is a complex area of study. In some cases, COPD can lead to the development of fibrotic changes in the lung. Conversely, the presence of fibrosis can exacerbate COPD symptoms. This interplay suggests a potential overlap in pathophysiological mechanisms, such as chronic inflammation and immune response dysregulation.
Part 3: Advances in Clinical Trials
Recent clinical trials have focused on developing treatments that target the underlying mechanisms of both COPD and Pulmonary Fibrosis. These trials are exploring novel therapeutic agents, including anti-inflammatory drugs, antifibrotic agents, and biologics. The design of these trials, often involving large patient cohorts and long-term follow-up, is crucial in understanding the efficacy and safety of these new treatments.
Breakthroughs in Drug Development
Innovations in drug development for COPD and Pulmonary Fibrosis focus on targeting specific molecular pathways involved in disease progression. Recently, trials on new classes of bronchodilators and anti-inflammatory agents have shown promise in improving lung function and reducing flare-ups in COPD patients. For Pulmonary Fibrosis, antifibrotic drugs like nintedanib and pirfenidone have been groundbreaking, significantly slowing disease progression.
Analysis of Trial Designs and Outcomes
Clinical trials in this field are increasingly adopting sophisticated designs like adaptive and multi-arm trials to efficiently assess the effectiveness of multiple treatments. Patient-centric outcomes, such as quality of life and symptom reduction, are becoming primary endpoints alongside traditional measures like lung function and survival rates.
Part 4: Emerging Therapies and Future Directions
Gene Therapy and Personalized Medicine
The future of COPD and Pulmonary Fibrosis treatment lies in personalized medicine and gene therapy. Ongoing research is exploring genetic markers that could predict disease progression and response to treatment. Gene therapies aim to target these specific genetic factors to halt or reverse lung damage.
Stem Cell Therapy and Regenerative Medicine
Stem cell therapy offers a novel approach to potentially regenerate damaged lung tissue. Clinical trials are underway to understand the safety and efficacy of stem cell transplants in lung disease patients.
Innovations in Non-pharmacological Treatments
Beyond medications, there’s growing interest in non-pharmacological interventions like specialized pulmonary rehabilitation programs, dietary modifications, and the use of digital health tools to monitor and manage these conditions.
Conclusion
COPD and Pulmonary Fibrosis represent significant challenges in pulmonary medicine. While recent advances in clinical trials and emerging therapies offer hope, there is still much to learn about these complex diseases. Ongoing research, patient-centric approaches, and collaborative efforts are key to developing more effective treatments and improving the lives of those affected.